What you should know about AFib
Produced by:
In medicine, AFib is not an exaggeration of the truth. Rather, it is an abbreviation for atrial fibrillation, the most common type of arrhythmia — or abnormal heart rhythm. AFib results from disorganization of the heart’s electricity that can cause an irregular heartbeat. Many people are not aware the condition has serious consequences such as an estimated four- to five-fold increased risk of ischemic stroke.
Electrical signals sent between the chambers of the heart, through its conduction system, tell each part when and how to beat. Normally, the top chambers of the heart—or atria—beat first, initiated by an impulse that starts in a small area of the right atrium. Then, the bottom chambers — or ventricles, pump blood out to the body.1 With Afib, the upper and lower chambers do not beat in a coordinated way. This may occur as a result of problems with the conduction system including the initial impulse not starting in the right place or when there’s an abnormal flow of the electrical current.2,3 These abnormalities can result in an irregular, disorganized, and often fast heartbeat. When this happens, the ventricles do the best they can to keep up, but instead, they pump irregularly and often very fast, preventing blood from being pumped as well as it should. This leads to a higher risk of blood clots, stroke, heart failure, other cardiac complications and even death.
Symptoms of AFib include palpitations, fluttering or thumping in the chest, heart racing, and dizziness or passing out if the pumping function of the heart is affected. Other symptoms can include chest pain, shortness of breath and extreme fatigue.4 Since the irregular rhythm makes it hard for blood to flow effectively, the slow flow can make the heart prone to form blood clots. If blood clots break off, they can be pumped out of the heart and clog a blood vessel meant to supply oxygen to various parts of the body. If this occurs in the brain, that part of the brain can die — causing a stroke. Patients with aFib are at an increased risk for a stroke.5 Around 15-20% of people who have suffered from a straoke have Afib.1 Importantly, AFib is not always symptomatic. In people without obvious symptoms, AFib is only detectable upon physical examination or with monitoring the heart rhythm.
Some risk factors for AFib can be modified while others cannot. Non-modifiable risk factors include advanced age, being male, underlying heart problems, history of prior heart surgery and genetics. Modifiable risk factors include lifestyle changes such as limiting alcohol intake, prevention/treatment of obstructive sleep apnea and good control of chronic conditions like hypertension, diabetes, asthma, obesity and thyroid problems. Additionally, athletes are at risk for by Afib, which can be triggered by a rapid increase of their heart rate (supraventricular tachycardia).6
People of European descent are more likely to have aFib than their black counterparts and since women generally live longer, and having Afib increases with age, women are more likely to have AFib than men.4
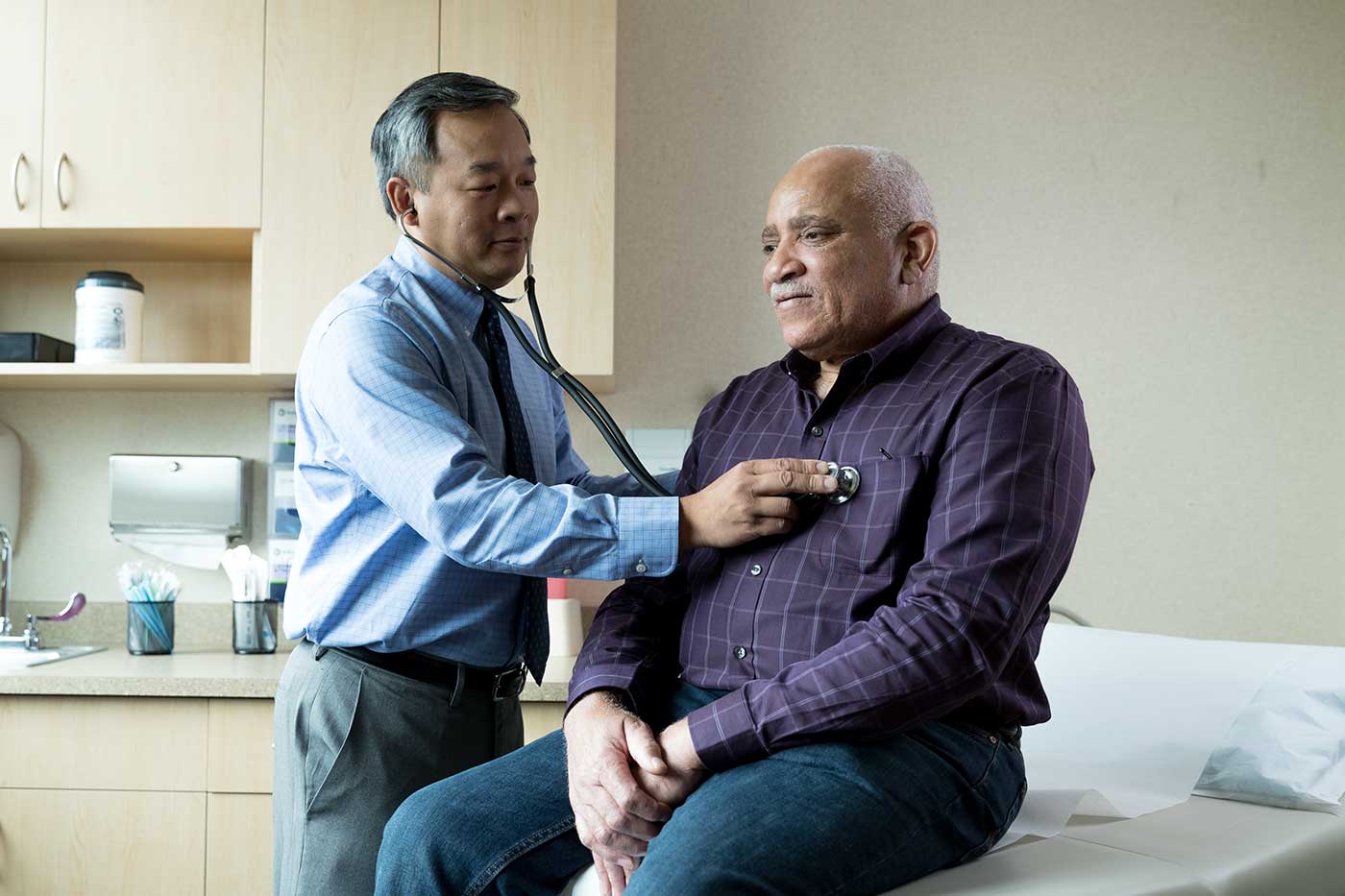
The key to avoiding the long-term issues caused by AFib is to have an early diagnosis and begin a treatment plan that is right for you. If your primary care doctor or cardiologist suspects you have AFib, he or she may refer you to a cardiac electrophysiologist — or EP — for further evaluation. An EP can decide what the right approach might be to properly diagnose and manage AFib.
AFib treatment options include:
- Medications that control the heart’s rate to keep it from beating too fast, or other medicines that work to try to normalize the heart rhythm and keep it out of Afib. Most will need to take anticoagulants — or blood thinners — in order to lower their risk of stroke from AFib in addition to continuing treatments that work to maintain good heart rhythm.
- Cardioversion resets the heart rhythm and converts it out of AFib back to the normal rhythm. This can be done with pills or intravenous medications but is more commonly done by sedating the patient with anesthesia and shocking the heart back into rhythm.
- Ablation is a low-risk, catheter-based procedure, which involves mapping the electricity of the parts of the heart where AFib often originates and isolating those areas using special catheters and technology.7Patients will often use a combination of these therapies to treat Afib. Since atrial fibrillation is a chronic disease, it is important for those affected to follow their treatment plan. Proper diagnosis and treatment of AFib can have a huge impact on quality of life.
If you believe you are suffering from symptoms of Afib, our expert and board-certified cardiologists at Optum Medical Care can help diagnose your condition and provide a personalized treatment plan. To learn more, schedule an appointment or find a physician.
Disclaimer:
The information featured in this site is general in nature. The site provides health information designed to complement your personal health management. It does not provide medical advice or health services and is not meant to replace professional advice or imply coverage of specific clinical services or products. The inclusion of links to other web sites does not imply any endorsement of the material on such websites.
- How the Heart Works. https://www.nhlbi.nih.gov/health/heart/heart-beats. Last updated March 24, 2022. Accessed June 1, 2023.
- Why Atrial Fibrillation Matters. https://www.heart.org/en/health-topics/atrial-fibrillation/why-atrial-fibrillation-af-or-afib-matters. Last reviewed March 24, 2023. Accessed June 1, 2023.
- What Is Atrial Fibrillation? https://www.nhlbi.nih.gov/health/atrial-fibrillation. Last updated November 30, 2022. Accessed June 1, 2023.
- Atrial Fibrillation. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm. Last review October 14, 2022. Accessed May 2, 2023.
- What is Atrial Fibrillation (AFib or AF)? https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af. Revised March 23, 2023. Accessed May 1, 2023.
- Who is at Risk for Atrial Fibrillation? https://www.heart.org/en/health-topics/atrial-fibrillation/who-is-at-risk-for-atrial-fibrillation-af-or-afib. Last reviewed March 24, 2023. Accessed June 1, 2023.
- Cardiac ablation procedures. https://medlineplus.gov/ency/article/007368.htm. Last reviewed October 5, 2022. Accessed June 1, 2023.
Getting to the heart of postural orthostatic tachycardia syndrome (POTS)
Getting to the heart of postural orthostatic tachycardia syndrome (POTS)
Read articleHealthy habits to help stop bladder leaks
Learn how to regain control of your bladder and avoid accidents.
Read articleShould you get tested for seasonal allergies?
Pollen allergies happen in the fall, too. If you’ve got a runny nose and itchy eyes, you may need to see a doctor.
Read article
